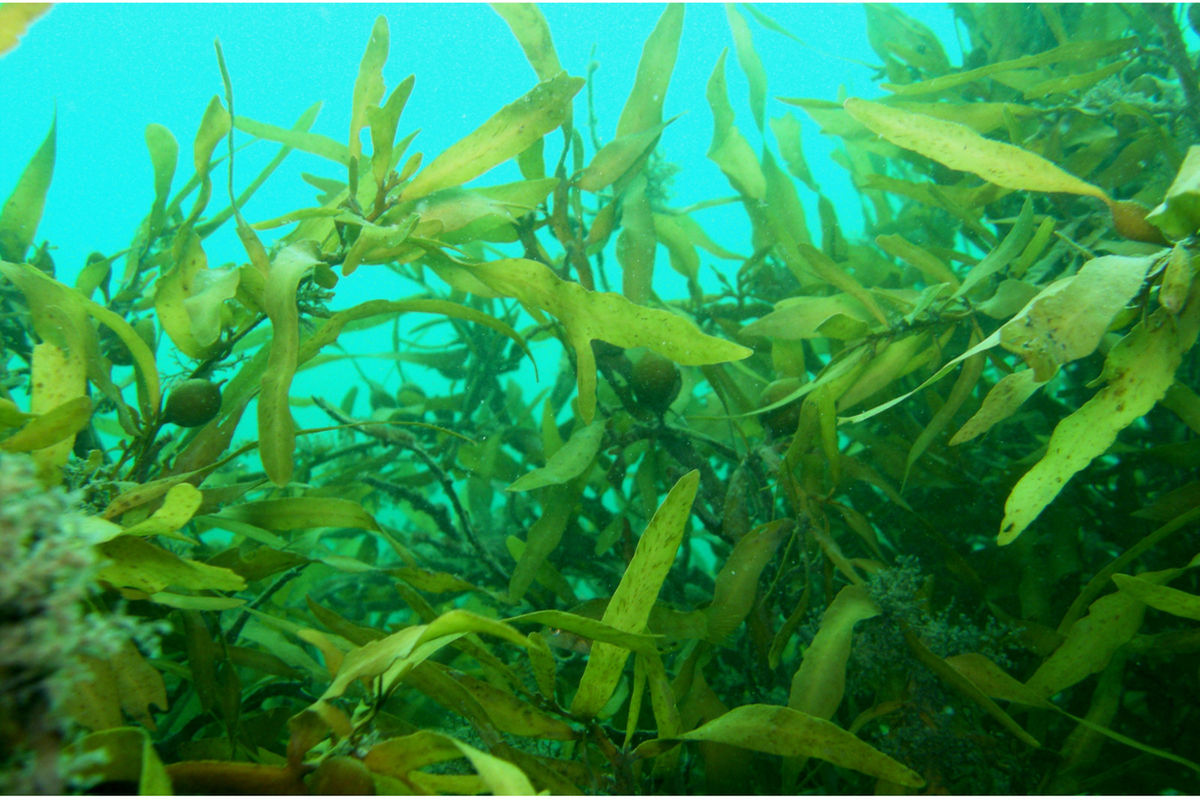
Dar es Salaam. NMB Bank has signed a Memorandum of Understanding (MoU) with state-owned Zanzibar Seaweed Company (Zasco) that could significantly unlock the potential for seaweed farming in Zanzibar.
NMB Bank Chief of Retail Banking Filbert Mponzi said at the MoU signing ceremony in Dar es Salaam at the weekend that the move aligns with the bank’s ambitious strategy of supporting sustainable economic development in Zanzibar.
Mr Mponzi said NMB has been at the forefront of supporting Zanzibar’s Blue Economy agenda and that signed MoU with Zasco will help in value addition and also in increasing the Isles’ foreign exchange earnings.
“This MoU reaffirms our commitment to supporting Zanzibar’s Blue Economy agenda. Our biggest role will be to increase the efficiency of smallholder seaweed farmers in Zanzibar by providing tailor-made banking products, financial literacy as well as technical training right at grassroots level,” Mponzi said.
Earlier, the Zasco Director General Dr Masoud Rashid Mohammed noted that the MoU had come at an opportune time as the company is embarking on its strategy to boost value addition in seaweed farming.
“We believe this MoU will be a game-changer. We will do everything possible to implement all the terms stipulated on time,” Mohamed said.
Mohamed said his company has already commenced construction of an Sh 8 billion seaweed processing plant in Zanzibar that will ensure that all the seaweed is processed before export so as to enable farmers to fetch better prices at the world market.
“This will be the biggest seaweed processing plant not only in Tanzania but Africa as a whole. Indeed this MoU has come timely as the production capacity of seaweed is still very low,” he said.
The Zanzibar Trade and Industrial Development Minister Omar Said Shabani during the event expressed optimism that seaweed is poised to overtake cloves as Zanzibar’s biggest foreign exchange earner within a few years to come.
“The price of seaweed is higher than that of cloves at the world market. With ample investment especially in value addition for seaweed, Zanzibar will be in position to get more foreign exchange,” he said.
Shabani said Zanzibar produces 23,000 tonnes of seaweed per annum with 90 percent of the out growers being women.